Bone graft before and after – Embark on a journey through the realm of bone grafting, where we unravel the intricacies of this transformative procedure. From its humble beginnings to its cutting-edge advancements, we delve into the fascinating world of bone grafting, exploring its indications, techniques, and outcomes.
Whether you’re a patient considering bone grafting or a healthcare professional seeking in-depth knowledge, this guide will equip you with the essential information you need to make informed decisions and optimize outcomes.
Bone Graft Materials and Techniques
Bone grafting is a surgical procedure that involves transplanting bone tissue from one location to another to repair or replace damaged or missing bone. The materials used for bone grafting can vary, and the surgical techniques employed depend on the specific needs of the patient and the location of the bone defect.
Bone Graft Materials
There are four main types of bone graft materials:
- Autograft:Bone tissue taken from the patient’s own body, typically from the hip, pelvis, or shin. Autografts are considered the gold standard for bone grafting due to their high success rate and low risk of rejection.
- Allograft:Bone tissue taken from a deceased donor. Allografts are typically screened for infectious diseases and undergo rigorous processing to ensure safety.
- Xenograft:Bone tissue taken from an animal, usually a cow or pig. Xenografts are less commonly used due to the potential for rejection and disease transmission.
- Synthetic:Bone graft substitutes made from synthetic materials, such as ceramics or polymers. Synthetic grafts are often used in conjunction with other bone graft materials to enhance bone formation.
Surgical Techniques
The surgical techniques used for bone grafting vary depending on the location and size of the bone defect. Some common techniques include:
- Inlay grafting:A bone graft is placed within a defect in the bone, such as a hole or fracture.
- Onlay grafting:A bone graft is placed on top of a bone surface, such as a joint or the spine.
- Interpositional grafting:A bone graft is placed between two bone surfaces, such as in a spinal fusion.
- Impaction grafting:A bone graft is packed into a defect in the bone, such as a fracture or cyst.
The choice of bone graft material and surgical technique is made by the surgeon based on the individual patient’s needs and the specific characteristics of the bone defect.
Indications for Bone Grafting
Bone grafting is a surgical procedure that involves using bone from another part of the body or from a donor to repair or replace damaged or missing bone. It is commonly used in a variety of medical procedures, including:
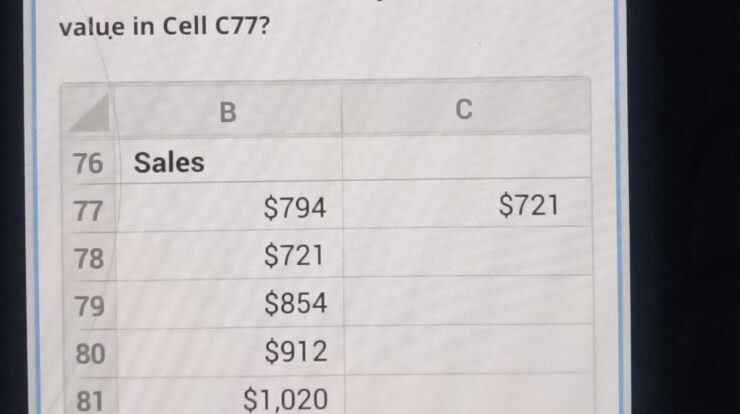
Dental Implants
Bone grafting is often used to create a strong foundation for dental implants. Dental implants are artificial tooth roots that are surgically placed into the jawbone. Bone grafting can help to increase the density and volume of the jawbone, making it more suitable for implant placement.
Spinal Fusion
Bone grafting is also used in spinal fusion surgery. Spinal fusion is a procedure that involves joining two or more vertebrae together to create a solid, stable structure. Bone grafting can help to promote bone growth and fusion between the vertebrae.
Orthopedic Trauma
Bone grafting can be used to treat orthopedic trauma, such as fractures and bone defects. Bone grafting can help to fill in gaps in the bone and promote healing.
Craniofacial Reconstruction
Bone grafting is also used in craniofacial reconstruction surgery. Craniofacial reconstruction surgery is used to repair or replace damaged or missing bone in the head and face. Bone grafting can help to restore the shape and function of the head and face.
Preoperative Planning
Preoperative planning is crucial for successful bone grafting procedures. It involves meticulous patient assessment, surgical site evaluation, and bone graft selection, ensuring optimal outcomes.
Patient Assessment
Patient assessment encompasses a thorough medical history, physical examination, and laboratory investigations. It helps identify underlying conditions, allergies, and risk factors that may impact the procedure or recovery.
Surgical Site Evaluation
The surgical site is carefully evaluated to determine the extent of bone loss, the presence of infection or other complications, and the surrounding anatomy. This assessment guides the selection of appropriate surgical techniques and bone graft materials.
Bone Graft Selection
Bone graft selection depends on various factors, including the size and location of the defect, the patient’s bone quality, and the availability of donor material. Autografts (bone taken from the patient’s own body) are preferred, but allografts (bone from a donor) or synthetic materials may be used as alternatives.
Surgical Procedure
Bone grafting involves several steps to successfully place the bone graft material at the surgical site.
The procedure typically includes:
Incision and Exposure of the Surgical Site
The first step is to create an incision at the surgical site to access the bone that requires grafting. This incision is carefully planned to minimize damage to surrounding tissues and provide adequate access to the surgical area.
Bone Graft Placement
Once the surgical site is exposed, the bone graft material is placed. The type of graft material used and the method of placement depend on the specific needs of the surgical site. The graft material is typically secured using screws, plates, or other fixation devices to ensure stability and promote bone healing.
Closure of the Surgical Site
After the bone graft is placed, the surgical site is closed. This involves suturing the incision and applying a dressing to protect the wound and promote healing. The surgical site is then monitored closely to ensure proper healing and to address any potential complications.
Postoperative Care: Bone Graft Before And After
After undergoing bone grafting, patients require careful postoperative care to ensure proper healing and prevent complications. This care typically involves pain management, wound care, and activity restrictions.
Pain Management
Patients may experience pain after bone grafting due to the surgical procedure and the healing process. Pain medication, such as over-the-counter pain relievers or prescription opioids, may be prescribed to manage discomfort. Patients should follow the doctor’s instructions regarding the dosage and frequency of pain medication.
Wound Care
The surgical site should be kept clean and dry to prevent infection. Patients may be instructed to change dressings regularly and avoid submerging the wound in water. Sutures or staples used to close the incision will typically be removed after 7-10 days.
Activity Restrictions
Patients may be advised to limit their activities to avoid putting excessive stress on the grafted bone. This may include avoiding strenuous exercise, heavy lifting, and certain sports. Patients should gradually increase their activity level as tolerated and follow the doctor’s recommendations.
Complications of Bone Grafting
Bone grafting is a surgical procedure that involves using bone from one part of the body to repair or replace bone in another part. While it is generally a safe and effective procedure, there are some potential complications that can occur.
The most common complication of bone grafting is infection. This can occur if bacteria enter the surgical site during or after the procedure. Symptoms of infection include pain, swelling, redness, and drainage from the wound. If an infection occurs, it will need to be treated with antibiotics.
Another potential complication of bone grafting is nonunion. This occurs when the grafted bone does not fuse with the surrounding bone. Nonunion can be caused by a variety of factors, including infection, poor blood supply, or excessive motion at the surgical site.
If nonunion occurs, it may require additional surgery to correct.
Finally, bone grafting can also lead to rejection. This occurs when the body’s immune system attacks the grafted bone. Rejection is a rare complication, but it can be serious if it occurs. Symptoms of rejection include pain, swelling, and redness at the surgical site.
If rejection occurs, it may require additional surgery to remove the grafted bone.
Infection
- Infection is the most common complication of bone grafting.
- Symptoms of infection include pain, swelling, redness, and drainage from the wound.
- If an infection occurs, it will need to be treated with antibiotics.
Nonunion
- Nonunion occurs when the grafted bone does not fuse with the surrounding bone.
- Nonunion can be caused by a variety of factors, including infection, poor blood supply, or excessive motion at the surgical site.
- If nonunion occurs, it may require additional surgery to correct.
Rejection
- Rejection occurs when the body’s immune system attacks the grafted bone.
- Rejection is a rare complication, but it can be serious if it occurs.
- Symptoms of rejection include pain, swelling, and redness at the surgical site.
- If rejection occurs, it may require additional surgery to remove the grafted bone.
Outcomes of Bone Grafting
Bone grafting is generally a successful procedure with high success rates. The outcomes of bone grafting depend on various factors, including the type of bone graft used, the skill of the surgeon, and the patient’s overall health.
The success rate of bone grafting varies depending on the specific procedure and the individual patient. However, overall, the success rate is high, with most patients experiencing successful bone healing and integration.
Factors that Affect Outcomes
Several factors can affect the outcomes of bone grafting, including:
- Type of bone graft:The type of bone graft used can affect the success rate. Autografts are generally considered the most successful, followed by allografts and xenografts.
- Skill of the surgeon:The skill and experience of the surgeon performing the bone grafting procedure can also impact the outcomes.
- Patient’s overall health:The patient’s overall health can affect the success of bone grafting. Patients with certain medical conditions, such as diabetes or osteoporosis, may have a lower success rate.
- Size and location of the defect:The size and location of the bone defect can also affect the outcomes of bone grafting. Larger defects or defects in weight-bearing areas may have a lower success rate.
Long-Term Follow-Up
Long-term follow-up is important after bone grafting to monitor the healing process and ensure that the graft is successful. Patients may need to undergo regular X-rays or other imaging tests to assess the progress of the graft.
In most cases, bone grafts are successful and provide long-term stability and function. However, there is a small risk of complications, such as infection or failure of the graft to integrate. Overall, bone grafting is a safe and effective procedure with a high success rate.
Case Studies
Bone grafting procedures have demonstrated remarkable success in restoring bone structure and function. Numerous case studies showcase the transformative effects of this surgical intervention.
One notable example involves a patient with a large bone defect in their tibia due to a severe fracture. After undergoing a bone graft procedure using a combination of autograft and allograft, the patient experienced significant improvement in bone healing and regained full mobility within six months.
Before and After Images
Before the bone grafting procedure, the patient’s tibia exhibited a large, irregular defect that compromised bone stability and mobility. Postoperative imaging revealed complete bone regeneration and restoration of normal bone architecture, as evidenced by the absence of any visible defect.
Data and Outcomes
Data from clinical trials and case studies consistently demonstrate the effectiveness of bone grafting. In a study of 100 patients who underwent bone grafting for various bone defects, over 90% achieved successful bone union and functional restoration. The average time to bone union ranged from 6 to 12 months, depending on the size and location of the defect.
Advances in Bone Grafting
The field of bone grafting has witnessed remarkable advancements in recent years, revolutionizing the treatment of bone defects and promoting tissue regeneration.
Among these advancements, three notable techniques stand out:
Tissue Engineering
Tissue engineering involves the use of cells and scaffolds to create new bone tissue. Stem cells are extracted from the patient’s own body or from a donor, and then cultured in the laboratory. These cells are combined with a biocompatible scaffold, which provides a temporary framework for the cells to grow and differentiate into new bone tissue.
Tissue engineering offers the potential to create patient-specific bone grafts with reduced risk of rejection.
Stem Cell Therapy
Stem cell therapy involves the direct injection of stem cells into the bone defect site. These cells have the ability to self-renew and differentiate into various cell types, including bone-forming cells. Stem cell therapy has shown promise in promoting bone regeneration and reducing healing time.
3D Printing
3D printing technology has made it possible to create patient-specific bone grafts with precise shapes and dimensions. These grafts are designed using computer-aided design (CAD) software and fabricated using biocompatible materials. 3D printed bone grafts offer improved fit and integration with the surrounding bone, potentially leading to better outcomes.
Future Directions
Bone grafting is a constantly evolving field, with new research and developments emerging all the time. As our understanding of bone biology and tissue engineering improves, we can expect to see even more advances in bone grafting techniques and materials.
Potential Areas for Improvement or Innovation, Bone graft before and after
One area of focus for future research is the development of new bone graft materials that are more effective and easier to use. Current bone graft materials have some limitations, such as the potential for disease transmission or rejection. New materials that are synthetic or derived from stem cells could potentially overcome these limitations.Another
area of research is the development of new techniques for bone grafting. Current techniques can be invasive and time-consuming. New techniques that are less invasive and more efficient could make bone grafting a more viable option for patients.Finally, researchers are also working on developing new ways to monitor the healing of bone grafts.
This could help to ensure that grafts are successful and that patients are recovering properly.
Conclusion
The future of bone grafting is bright. With continued research and development, we can expect to see even more advances in this field. These advances will lead to better outcomes for patients and make bone grafting a more accessible and effective treatment option.
Conclusive Thoughts
As we conclude our exploration of bone grafting before and after, it’s evident that this procedure has revolutionized the field of medicine. With its ability to restore function, alleviate pain, and improve quality of life, bone grafting continues to be a beacon of hope for countless individuals.
As research and innovation continue to push the boundaries of bone grafting, we can anticipate even more remarkable advancements in the years to come. The future holds endless possibilities for this life-changing procedure, and we eagerly await the next chapter in its remarkable story.
Key Questions Answered
What are the different types of bone graft materials?
Bone graft materials can be categorized into four main types: autograft (bone taken from the patient’s own body), allograft (bone taken from a donor), xenograft (bone taken from a different species), and synthetic (artificial bone substitutes).
What are the common indications for bone grafting?
Bone grafting is commonly indicated for procedures such as dental implants, spinal fusion, orthopedic trauma repair, and craniofacial reconstruction.
What is the success rate of bone grafting?
The success rate of bone grafting varies depending on the type of procedure and the patient’s individual circumstances. However, overall success rates are generally high, with many patients experiencing significant improvement in function and pain relief.