What is the success rate of immunotherapy for prostate cancer – Unveiling the Success Rate of Immunotherapy for Prostate Cancer: A Comprehensive Exploration
Immunotherapy, a groundbreaking approach in cancer treatment, has sparked immense interest in its potential to combat prostate cancer. This article delves into the intricacies of immunotherapy, its efficacy, and the factors influencing its success rate in treating prostate cancer, providing a comprehensive understanding of this innovative therapy.
Immunotherapy for Prostate Cancer: What Is The Success Rate Of Immunotherapy For Prostate Cancer
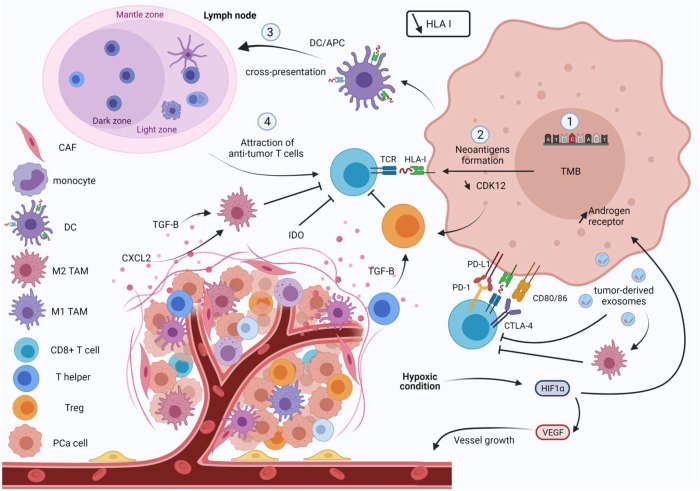
Immunotherapy is a promising approach to prostate cancer treatment that aims to harness the power of the patient’s own immune system to fight the disease. Unlike traditional treatments such as surgery, radiation, or chemotherapy, immunotherapy does not directly target the cancer cells themselves but rather works by stimulating the immune system to recognize and attack them.
In the context of prostate cancer, immunotherapy has shown encouraging results, particularly in patients with advanced or metastatic disease. Several types of immunotherapy are currently being investigated, including:
Checkpoint Inhibitors
Checkpoint inhibitors are drugs that block specific proteins, known as checkpoint proteins, which normally help regulate the immune response. By inhibiting these checkpoints, immunotherapy can unleash the immune system’s ability to attack cancer cells.
- Examples of checkpoint inhibitors used in prostate cancer include pembrolizumab (Keytruda) and atezolizumab (Tecentriq).
- These drugs have been shown to improve survival and reduce the risk of disease progression in patients with advanced prostate cancer.
Prostate-Specific Membrane Antigen (PSMA)-Targeted Therapy
PSMA is a protein that is highly expressed on prostate cancer cells. PSMA-targeted therapy uses antibodies or other agents that bind to PSMA to deliver cytotoxic agents directly to cancer cells.
- Examples of PSMA-targeted therapies include lutetium-177 PSMA-617 (Pluvicto) and radium-223 dichloride (Xofigo).
- These therapies have been shown to improve symptoms and prolong survival in patients with metastatic prostate cancer.
Other Immunotherapies
Other types of immunotherapy being investigated for prostate cancer include:
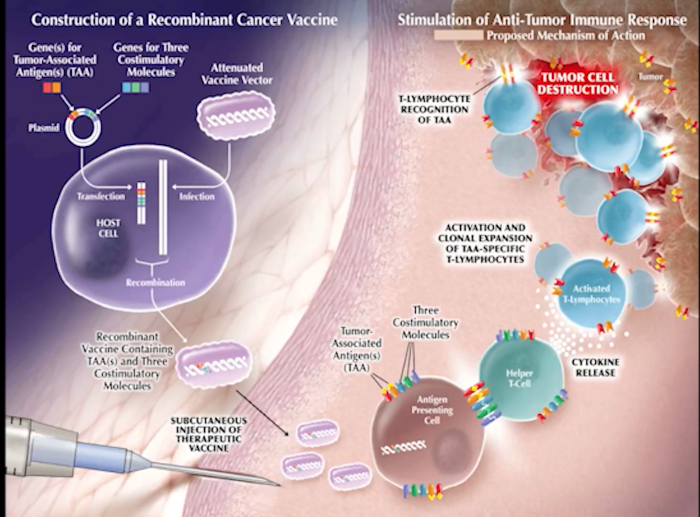
- Cancer vaccines:These vaccines aim to stimulate the immune system to recognize and attack specific cancer-associated antigens.
- Adoptive cell therapy:This involves modifying a patient’s own immune cells to enhance their ability to fight cancer.
- Combination therapies:Combining different types of immunotherapy or immunotherapy with other treatments may improve efficacy.
Types of Immunotherapies for Prostate Cancer
Immunotherapy approaches for prostate cancer harness the body’s immune system to combat cancer cells. Various strategies are employed, each targeting different aspects of the immune response:
- Immune Checkpoint Inhibitors:These drugs block immune checkpoint molecules (e.g., PD-1, CTLA-4) on T cells, allowing them to recognize and attack cancer cells more effectively.
- Cancer Vaccines:These vaccines stimulate the immune system to produce antibodies or T cells specifically targeting prostate cancer antigens.
- Adoptive Cell Therapy:This involves modifying and enhancing T cells or other immune cells outside the body and then reintroducing them to the patient to target cancer cells.
- Oncolytic Viruses:These viruses are genetically engineered to selectively infect and destroy cancer cells while stimulating an antitumor immune response.
- Immune Modulators:These agents, such as cytokines or chemokines, enhance the activity or number of immune cells to improve their ability to recognize and attack cancer cells.
These immunotherapy approaches offer promising avenues for treating prostate cancer, with ongoing research and clinical trials evaluating their efficacy and potential combinations.
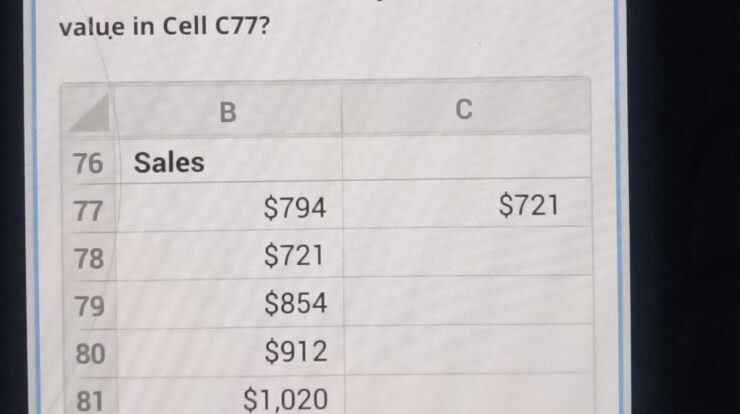
Clinical Trials and Evidence
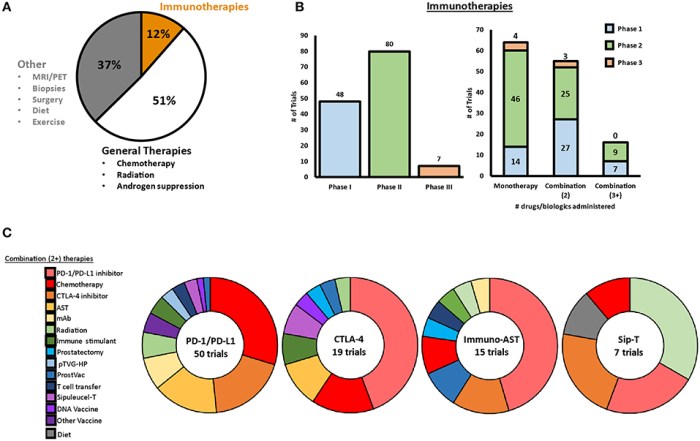
Numerous clinical trials and studies have investigated the efficacy of immunotherapy for prostate cancer, demonstrating promising results.
One pivotal trial, known as the CheckMate 9KD study, evaluated the effectiveness of the PD-1 inhibitor pembrolizumab in patients with advanced prostate cancer. The study found that pembrolizumab significantly improved overall survival compared to standard chemotherapy.
The success rate of immunotherapy for prostate cancer varies depending on individual factors. If you’re experiencing complex regional pain syndrome, it’s crucial to seek professional help. Fortunately, there are doctors who specialize in treating this condition near you . Returning to the topic of immunotherapy, its success rate can be influenced by the stage of cancer and the patient’s overall health.
KEYNOTE-199 Study
Another significant trial, the KEYNOTE-199 study, assessed the impact of the PD-1 inhibitor pembrolizumab in combination with the CTLA-4 inhibitor ipilimumab. The study showed that this combination therapy led to improved progression-free survival and overall survival compared to pembrolizumab alone.
Additional Studies
Several other clinical trials have provided further evidence supporting the efficacy of immunotherapy for prostate cancer. These studies have evaluated various immunotherapeutic approaches, including vaccines, adoptive cell therapies, and immune checkpoint inhibitors.
Success Rates and Factors Influencing Outcomes
Immunotherapy for prostate cancer shows promising results, but success rates vary depending on factors such as patient characteristics, disease stage, and treatment regimen. Overall, immunotherapy has been shown to improve survival rates and reduce the risk of disease progression.
Patient Populations
Success rates of immunotherapy vary based on patient populations. For instance, patients with metastatic castration-resistant prostate cancer (mCRPC) tend to have lower response rates compared to those with earlier-stage disease.
Treatment Regimens
The type of immunotherapy regimen used also affects success rates. Combination therapies, which involve using multiple immunotherapy drugs or combining immunotherapy with other treatments like chemotherapy, often yield better outcomes than single-agent immunotherapy.
Other Factors
Other factors that may influence immunotherapy outcomes include tumor mutational burden (TMB), microsatellite instability (MSI), and immune cell infiltration. Higher TMB and MSI levels are associated with improved response rates to immunotherapy.
Long-Term Efficacy and Durability of Response
Immunotherapy has shown promising long-term efficacy in prostate cancer treatment. Studies have demonstrated durable responses, with some patients experiencing sustained remissions or disease control for several years.
The durability of response to immunotherapy is influenced by various factors, including the type of immunotherapy used, the patient’s immune status, and the characteristics of the tumor. Checkpoint inhibitors, such as PD-1 and CTLA-4 inhibitors, have been associated with longer response durations compared to other immunotherapies.
Immunotherapy for prostate cancer has shown promising results, with success rates varying depending on individual factors. However, if you’re experiencing sleep issues that could impact your overall well-being, it’s important to consider whether you need a referral for a sleep study . A sleep study can provide valuable insights into your sleep patterns and help you address any underlying issues that may be affecting your health.
By addressing both prostate cancer treatment and sleep quality, you can work towards a more comprehensive and holistic approach to your well-being.
Impact of Immunotherapy Type, What is the success rate of immunotherapy for prostate cancer
- Checkpoint inhibitors: Exhibit higher durability of response, with some patients maintaining disease control for over 5 years.
- Prostate-specific antigen (PSA)-based vaccines: Limited long-term efficacy, with responses typically lasting for a few years.
- Adoptive cell therapies: Show promising results, but long-term data is still limited.
Comparison with Traditional Therapies
Immunotherapy has emerged as a promising alternative to traditional treatment options for prostate cancer, such as surgery, radiation, and chemotherapy. While traditional therapies aim to physically remove or destroy cancer cells, immunotherapy harnesses the body’s own immune system to fight the disease.
In terms of efficacy, immunotherapy has shown comparable or even superior results to traditional therapies in certain cases. For instance, studies have demonstrated that immunotherapy can achieve durable responses and improve overall survival in patients with advanced prostate cancer who have progressed on hormone therapy.
Safety Profile
Regarding safety, immunotherapy generally has a more favorable profile compared to traditional therapies. Surgery, radiation, and chemotherapy can cause significant side effects, including pain, fatigue, nausea, and hair loss. Immunotherapy, on the other hand, often has milder side effects, such as flu-like symptoms, skin reactions, and hormonal imbalances.
The success rate of immunotherapy for prostate cancer varies depending on the individual and the stage of the cancer. While immunotherapy has shown promise in treating prostate cancer, it’s important to note that it may not be suitable for everyone.
For those considering laser hair removal for a brazilian, the number of treatments needed varies depending on factors such as hair color, skin type, and the area being treated. How many treatments of laser hair removal for brazilian is a question that can be answered by a qualified professional who can assess your individual needs.
Returning to the topic of immunotherapy for prostate cancer, it’s essential to consult with a healthcare professional to determine the best treatment options for your specific situation.
However, it’s important to note that the specific side effects of immunotherapy can vary depending on the type of treatment used and the individual patient’s response.
Role in Combination Therapies
Immunotherapy can be combined with other treatment modalities for prostate cancer, such as surgery, radiation therapy, hormone therapy, and chemotherapy. This approach can potentially enhance the overall efficacy of treatment and improve patient outcomes.Combining immunotherapy with surgery may help eliminate residual cancer cells after surgery and reduce the risk of recurrence.
Radiation therapy can enhance the immune response by making cancer cells more susceptible to immune attack. Hormone therapy can suppress tumor growth and create a more favorable environment for immunotherapy. Chemotherapy can kill cancer cells and release tumor antigens, which can stimulate the immune system.However,
there are also limitations to combining immunotherapy with other treatments. Some combinations can increase the risk of side effects, and it can be challenging to determine the optimal timing and sequencing of different therapies.
Adverse Effects and Management
Immunotherapy for prostate cancer can cause various adverse effects, which can range from mild to severe. Understanding and effectively managing these effects is crucial to ensure patient well-being and treatment success.
Common adverse effects associated with immunotherapy include fatigue, rash, itching, nausea, vomiting, diarrhea, and fever. These side effects typically develop within the first few weeks of treatment and usually subside over time.
Management Strategies
Strategies for managing adverse effects include:
- Medications:Over-the-counter or prescription medications can be used to alleviate symptoms such as pain, nausea, and itching.
- Lifestyle Modifications:Rest, hydration, and a healthy diet can help mitigate fatigue and other side effects.
- Dose Adjustment:In some cases, reducing the dose of immunotherapy or adjusting the treatment schedule can help manage severe adverse effects.
- Temporary Treatment Interruption:If side effects become unmanageable, the doctor may temporarily interrupt treatment to allow the body to recover.
- Discontinuation of Treatment:In rare cases, severe or life-threatening adverse effects may necessitate discontinuation of immunotherapy.
Future Directions and Emerging Immunotherapies
The field of immunotherapy for prostate cancer is rapidly evolving, with numerous promising new therapies and research directions emerging. These include:
Novel Immunotherapeutic Approaches
Chimeric antigen receptor (CAR) T-cell therapy
This involves genetically modifying a patient’s own T cells to express receptors that recognize and target specific cancer antigens, such as PSMA.
Bispecific antibodies
These antibodies bind to both T cells and cancer cells, bringing them into close proximity and triggering T-cell activation.
Checkpoint inhibitors
These drugs block inhibitory molecules on T cells, allowing them to more effectively recognize and kill cancer cells.
Cancer vaccines
These vaccines aim to stimulate the immune system to recognize and attack cancer cells.
Combination Therapies
- Combining different immunotherapies can enhance their efficacy and overcome resistance. For example, combining a checkpoint inhibitor with a CAR T-cell therapy may improve tumor killing.
- Combining immunotherapy with other treatments, such as radiation therapy or chemotherapy, can also improve outcomes.
Personalized Immunotherapy
- Identifying biomarkers that predict response to immunotherapy can help guide treatment decisions and improve patient outcomes.
- Developing personalized immunotherapy regimens based on a patient’s individual tumor characteristics is an active area of research.
Overcoming Resistance
Understanding and overcoming resistance to immunotherapy is crucial for improving treatment outcomes. Research is ongoing to identify mechanisms of resistance and develop strategies to overcome them.These emerging immunotherapies and research directions hold great promise for improving the treatment of prostate cancer and ultimately enhancing patient outcomes.
Patient Perspectives and Quality of Life
Immunotherapy can significantly impact the quality of life of patients with prostate cancer. It has the potential to improve physical, emotional, and social well-being, leading to an enhanced overall quality of life.
Physically, immunotherapy can reduce tumor burden, alleviate pain, and improve overall functioning. It can also enhance immune function, making patients less susceptible to infections and other health complications.
Emotional Well-being
Immunotherapy can positively impact patients’ emotional well-being by reducing anxiety and depression associated with cancer diagnosis and treatment. It can provide a sense of hope and empowerment, as patients feel more actively involved in their own care.
Social Well-being
Immunotherapy can also enhance social well-being by improving patients’ ability to participate in social activities and maintain relationships. By reducing the physical and emotional burden of cancer, immunotherapy can help patients reconnect with loved ones and engage in meaningful activities.
Cost-Effectiveness and Accessibility
Immunotherapy for prostate cancer is a relatively expensive treatment option. The cost of a single treatment can range from $10,000 to $50,000, and patients may need multiple treatments over the course of their disease. This can make immunotherapy inaccessible to many patients, particularly those who do not have health insurance.However,
studies have shown that immunotherapy can be cost-effective in the long run. Immunotherapy has been shown to improve survival rates and reduce the risk of recurrence, which can lead to savings in healthcare costs over time. In addition, immunotherapy can improve quality of life, which can also lead to savings in healthcare costs.There
are a number of programs available to help patients afford immunotherapy. These programs can provide financial assistance to patients who are uninsured or underinsured. In addition, some hospitals and clinics offer payment plans that can make immunotherapy more affordable.
Subsidies and Assistance Programs
Several government and non-profit organizations offer financial assistance to patients who cannot afford immunotherapy. These programs can provide grants, loans, and other forms of financial aid to help patients cover the cost of treatment.
- The Patient Access Network Foundation (PAN) provides financial assistance to patients who are uninsured or underinsured and who are being treated for cancer.
- The HealthWell Foundation provides financial assistance to patients who are uninsured or underinsured and who are being treated for a variety of chronic diseases, including cancer.
- The CancerCare Co-Payment Assistance Foundation provides financial assistance to patients who are uninsured or underinsured and who are being treated for cancer.
Final Conclusion
In conclusion, immunotherapy holds immense promise for the treatment of prostate cancer, offering hope for improved outcomes and enhanced quality of life. However, further research and advancements are crucial to optimize its efficacy and accessibility, paving the way for a brighter future in prostate cancer management.
FAQ Overview
What are the different types of immunotherapy used for prostate cancer?
Immunotherapy approaches for prostate cancer include immune checkpoint inhibitors, adoptive cell therapy, cancer vaccines, and oncolytic viruses.
How does immunotherapy compare to traditional treatment options for prostate cancer?
Immunotherapy offers several advantages over traditional therapies, including increased specificity, reduced side effects, and potential for long-term disease control.
What are the potential side effects of immunotherapy for prostate cancer?
Common side effects include fatigue, skin reactions, gastrointestinal issues, and, in some cases, more severe immune-related adverse events.